Researchers from Rice University and their partners have introduced an innovative method for destroying cancer cells, marking a significant advancement in oncology. This pioneering technique harnesses molecular vibrations induced by near-infrared light to effectively eliminate malignancies.
The breakthrough is centered around a small dye molecule frequently employed in medical imaging. When subjected to near-infrared light, these molecules create synchronized vibrations, known as plasmons, which result in the disruption of cancer cell membranes. This innovative process presents an alternative strategy for eliminating cancer cells without the use of conventional chemotherapy or radiation therapies.
Published in Nature Chemistry, the research demonstrated an impressive 99% success rate in eradicating lab-grown human melanoma cells. In mice with melanoma, 50% of treated individuals experienced complete remission, emphasizing the potential for this approach in future cancer treatments.

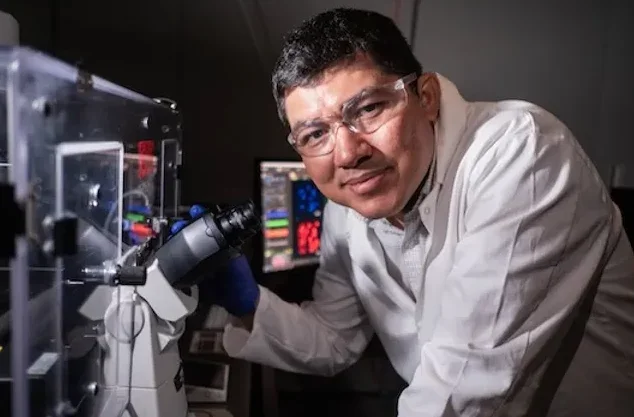
Chemist James Tour from Rice University dubbed these molecules “molecular jackhammers” for their rapid vibrational capabilities. His team had earlier developed nanoscopic structures featuring light-activated paddles that were effective in breaching the membranes of harmful bacteria, cancer cells, and drug-resistant pathogens.
Unlike the molecular motors invented by Nobel laureate Bernard Feringa, which function via a different approach, these molecular jackhammers operate at speeds exceeding one million times faster. Their responsiveness to near-infrared light signifies a substantial progress in molecular medicine.
A significant benefit of near-infrared light is its ability to penetrate deeply into human tissues without causing harm. Tour highlighted this attribute, noting that near-infrared light can reach depths of up to 10 centimeters (about 4 inches), while visible light only penetrates about half a centimeter (0.2 inches).
This deep penetration enhances the potential for molecular jackhammers in medical applications. Unlike traditional light-activated nano-tools, whose capabilities were limited by the short reach of visible light, this innovative method provides a more effective means of targeting tumors located deeper within the body.
The aminocyanine molecules behind this medical breakthrough are a specific class of synthetic dyes widely recognized in medical imaging.
These molecules possess impressive biocompatibility, water stability, and an affinity for attaching to the outer lipid layers of cells. Until this study, however, their potential as plasmons remained largely unexplored.
Ciceron Ayala-Orozco, the lead author, explained, “Due to their structure and chemical traits, the nuclei of these molecules can oscillate in unison when exposed to the appropriate stimulus. I recognized the need to harness the properties of plasmons for treatment and was intrigued by Dr. Tour’s mechanical strategy for addressing cancer cells. I essentially connected the dots.”
The researchers found that the molecular plasmons exhibited a near-symmetrical structure, with an arm that helped anchor the molecule to the lipid bilayer of the cell membrane, enhancing their effectiveness.

Importantly, the study clarified that this mechanism does not conform to the traditional categories of photodynamic or photothermal therapy. Ayala-Orozco emphasized, “This is the first time a molecular plasmon has been employed in such a manner to excite the entire molecule, generating mechanical action aimed at tearing apart the membrane of cancer cells.”
To gain better insight into the molecular characteristics driving this “jackhammering” effect, researchers from Texas A&M University, led by Jorge Seminario, conducted time-dependent density functional theory analyses.
The identification of molecular jackhammers represents a hopeful advancement in the continuous fight against cancer, offering a fresh method that targets cancer cells at a molecular level.
With its remarkable efficacy and minimal invasive nature, this discovery could drastically change cancer treatment, instilling renewed hope in patients and researchers alike. The scientific community now has new reasons to feel optimistic in the pursuit of a cancer cure.
Recent Innovations in Near-Infrared Light Applications in Medicine
Recent advancements utilizing near-infrared (NIR) light in medical fields are particularly promising, especially within diagnostics, imaging, and therapeutic contexts. Here are a few noteworthy developments:
Enhanced Tumor Imaging and Precision Therapy: Near-infrared light is being utilized for high-accuracy tumor imaging through fluorescent markers activated by NIR light. These markers enhance tumor visibility during surgical procedures, allowing surgeons to distinguish between cancerous and healthy tissue with exceptional precision. For instance, probes sensitive to NIR light are in development to target specific proteins or cancer markers, facilitating targeted treatment while minimizing damage to surrounding healthy tissues.

Non-Invasive Brain Imaging and Neurological Monitoring: Functional near-infrared spectroscopy (fNIRS) represents a new approach that employs NIR light to observe brain activity without invasive techniques. This technology enables real-time imaging of brain function, especially useful for detecting changes due to injuries or conditions such as epilepsy and stroke. It is gaining popularity as a more affordable, safer alternative to traditional imaging methods like fMRI, particularly for bedside monitoring.
Photobiomodulation Therapy (PBMT): NIR light is increasingly applied in PBMT to alleviate pain and inflammation while promoting wound healing and tissue regeneration. This approach is especially advantageous in managing chronic pain, enhancing recovery from sports injuries, and facilitating healing in patients with diabetes. The ability of PBMT using NIR wavelengths to penetrate deeply into tissues can significantly accelerate cellular repair.
Monitoring Blood Oxygen Levels in Newborns: Near-infrared spectroscopy is employed in neonatal intensive care to track blood oxygen levels in the brains and tissues of newborns. This non-invasive approach is essential for the early detection of hypoxia, a condition that can lead to serious neurological complications if not addressed promptly.

Targeted Drug Delivery and Controlled Release: Scientists are exploring NIR light as a means to trigger drug release in specific areas throughout the body. Certain engineered nanoparticles or hydrogels can be activated by NIR light to release medications, allowing precise control over the timing and location of drug delivery. This technique holds great promise for cancer treatment, enabling high doses to be directed at tumor sites with minimal impact on healthy tissues.
These innovative applications of NIR in medicine represent the forefront of clinical practice, using the deep tissue penetration and safety of near-infrared wavelengths to provide non-invasive, targeted, and patient-friendly diagnostic and therapeutic options.









