
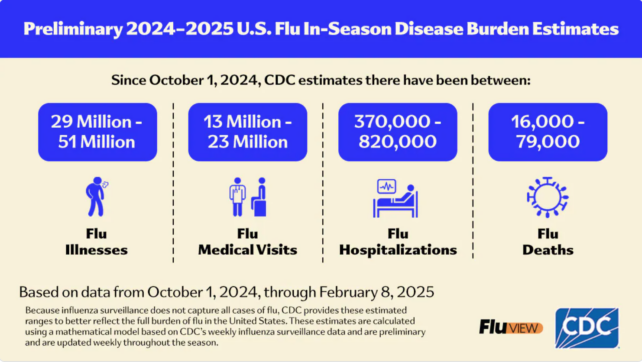
The United States is currently facing an unprecedented influenza outbreak that has affected between 29 and 51 million individuals and led to up to 820,000 hospitalizations since the onset of October.
This flu season ranks among the most severe in the past 15 years, with some experts attributing the rapid increase in cases to ‘vaccination fatigue’ induced by the post-COVID era and rampant misinformation. Prolonged discussions surrounding COVID-19 have likely contributed to increased vaccine hesitancy, undermining the public’s commitment to securing vaccinations for various health concerns.
The influenza A virus—distinct from the viruses that cause the common cold—appears to be capitalizing on this challenging climate.
According to the latest data from the Centers for Disease Control and Prevention (CDC), hospitals encountered over 50,000 patients battling this highly contagious respiratory disease in just one week this February.
The current flu season is classified by the CDC as “high severity“, marking the first instance of this classification since the 2017-2018 flu season.
CDC representative Paul Prince recently emphasized that anyone aged six months and older who has yet to receive the influenza vaccine this season “should get vaccinated without delay.”
Experts indicate that even at this stage of the flu season, it remains crucial for both children and adults to receive the vaccine to curb community transmission and enhance their chances of avoiding severe respiratory illness.
The CDC notes that recent estimates regarding the influenza outbreak are “preliminary, cumulative, and expected to rise as the season continues.”
Mortality rates related to influenza (primarily caused by influenza A) have already exceeded those attributed to COVID-19. In the week concluding February 8, 2.6 percent of all deaths were due to the flu, including 68 pediatric fatalities.
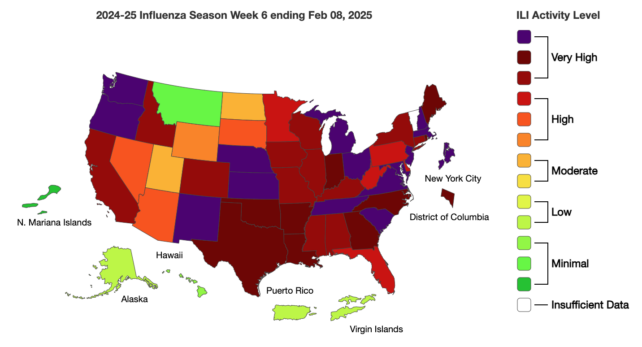
The CDC’s map of respiratory cases in healthcare settings reveals an alarming prevalence of flu activity across the nation, with shaded areas indicating extremely high levels of outpatient clinic visits as of February 8, 2025.
Only Montana, Alaska, and Hawaii remain in the green zone, while Vermont is unaccounted for due to inadequate data.
The reasons behind the sudden surge in influenza cases in the U.S. remain unclear; however, various interconnected factors likely contribute to this trend. For instance, this year’s flu vaccine may not be as effective against the circulating strains as in previous seasons, and vaccination rates have notably decreased since the COVID-19 pandemic emerged in 2020.
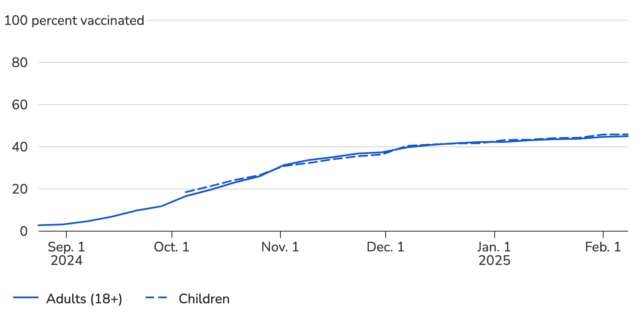
During the 2023-24 season, flu vaccination rates fell to their lowest point in 12 years. By the start of the 2024-25 season, only 37 percent of children in the U.S. had been vaccinated, marking a 6 percent decline from the prior year.
Adults are not faring much better; in November 2024, only around 35 percent of adults reported receiving a flu vaccine, despite many planning to obtain it later.
As of February, CDC data suggests that the majority of both children and adults in the U.S. have not yet received their annual influenza vaccination.
Flu vaccines have been in use for many years, and despite the rampant misinformation circulating online, they do not cause influenza. These vaccines work by stimulating the body to generate antibodies against various influenza virus strains, which are constantly evolving.
While seasonal flu vaccines may not completely prevent infection, they do significantly reduce the severity of illness and lower the risks of complications, hospitalization, and mortality.
Severe adverse effects from the flu vaccine, such as Guillain-Barré Syndrome, are exceedingly rare, occurring in about one in a million cases. In contrast, the vaccine saves tens of thousands of lives annually in the U.S., extending benefits beyond just those who receive it.
“Vaccination helps protect not only yourself but also those around you, particularly vulnerable populations like infants, elderly individuals, and those with chronic health issues,” according to the CDC
.
A 2022 study indicated that flu vaccines reduced a child’s chances of severe, life-threatening influenza by 75 percent.
If the public is experiencing fatigue from vaccine communications, it is vital for health authorities to explore new methods of highlighting the advantages of vaccination, particularly for vaccines that require ongoing updates, such as those for influenza and COVID-19.
Members of the American Academy of Family Physicians assert that family physicians are in a unique position to support their patients by engaging empathetically, providing evidence-based knowledge, and sharing personal stories to foster trust and encourage higher vaccination rates against influenza.
For further details on the 2024-2025 flu season, please visit the CDC website.









