
Dementia is often linked to significant memory impairment and a decline in cognitive abilities. This condition frequently presents alongside a range of psychiatric symptoms, including anxiety, sleep disturbances, and depression.
A recent population-based study conducted by researchers at the Karolinska Institute in Sweden reveals that a commonly prescribed group of medications for depression in dementia patients may be accelerating cognitive decline. Additionally, these medications could increase the likelihood of fractures and lead to a higher risk of premature death.
While other contributing factors cannot be entirely dismissed, it is crucial for healthcare providers to contemplate the potential adverse effects of certain antidepressants on patients with dementia.
Selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) are typically favored due to their relatively mild side effects. Nevertheless, recent findings have indicated a possible correlation between these medications and an elevated dementia risk among older adults in comparison to psychotherapy.
It is not surprising that certain categories of antidepressants may disrupt the cognitive processes necessary for memory and thinking. Despite this, SSRIs have often been regarded as beneficial in safeguarding the brain against neurodegeneration and are even associated with reducing the plaques believed to damage brain cells.
Efforts to reconcile these seemingly opposing results in the population have not yielded a definitive conclusion, possibly due to the nature of the data collected and inherent limitations in how the study was designed.
In their extensive analysis, neurobiologist Minjia Mo and her team at the Karolinska Institute utilized a national Swedish medical register, which included data from newly diagnosed dementia patients between 2007 and 2018. The study encompassed 18,740 patients, with over 20% having been recently prescribed at least one antidepressant.
Among these prescriptions, nearly two-thirds consisted of some type of SSRI.
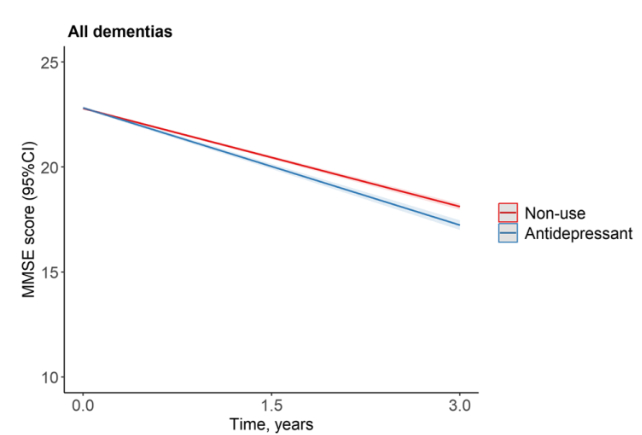
The researchers identified a clear connection between SSRIs and the exacerbation of dementia symptoms, noting that doses exceeding the standard daily recommendation corresponded with an increase of almost half a point annually in dementia assessment scores.
Due to the observational nature of the study, it is plausible that other variables may be influencing the observed relationship between the dosage of antidepressants and cognitive decline, making it challenging to establish clear causal links.
The interplay of existing cognitive decline among patients adds complexity to the analysis.
Additionally, the researchers noted a concerning increase in fracture risk associated with higher doses of SSRIs, suggesting potential adverse neurological implications, as well as indications of increased all-cause mortality.
No such association was found with SNRIs, hinting at potential differences in their mechanisms or possibly limitations in the study’s design. Future investigations may shed light on the benefits and risks associated with various classes of antidepressants.
It is essential to remember that any changes to medication should only be made under the guidance of a healthcare professional. Doctors and specialists in dementia care must evaluate a range of risks and possible benefits when creating treatment plans for individual patients and adjusting those plans as necessary.
Customizing medication combinations and dosages requires a thorough understanding of the patient’s overall prognosis, emphasizing the importance of studies like these in achieving the right balance to alleviate the distress associated with cognitive decline.
This research was published in BMC Medicine.









